Why the Name (and Approach) Has Changed
"It's not just a change in terminology — it's a complete shift in understanding how hip pain really works."
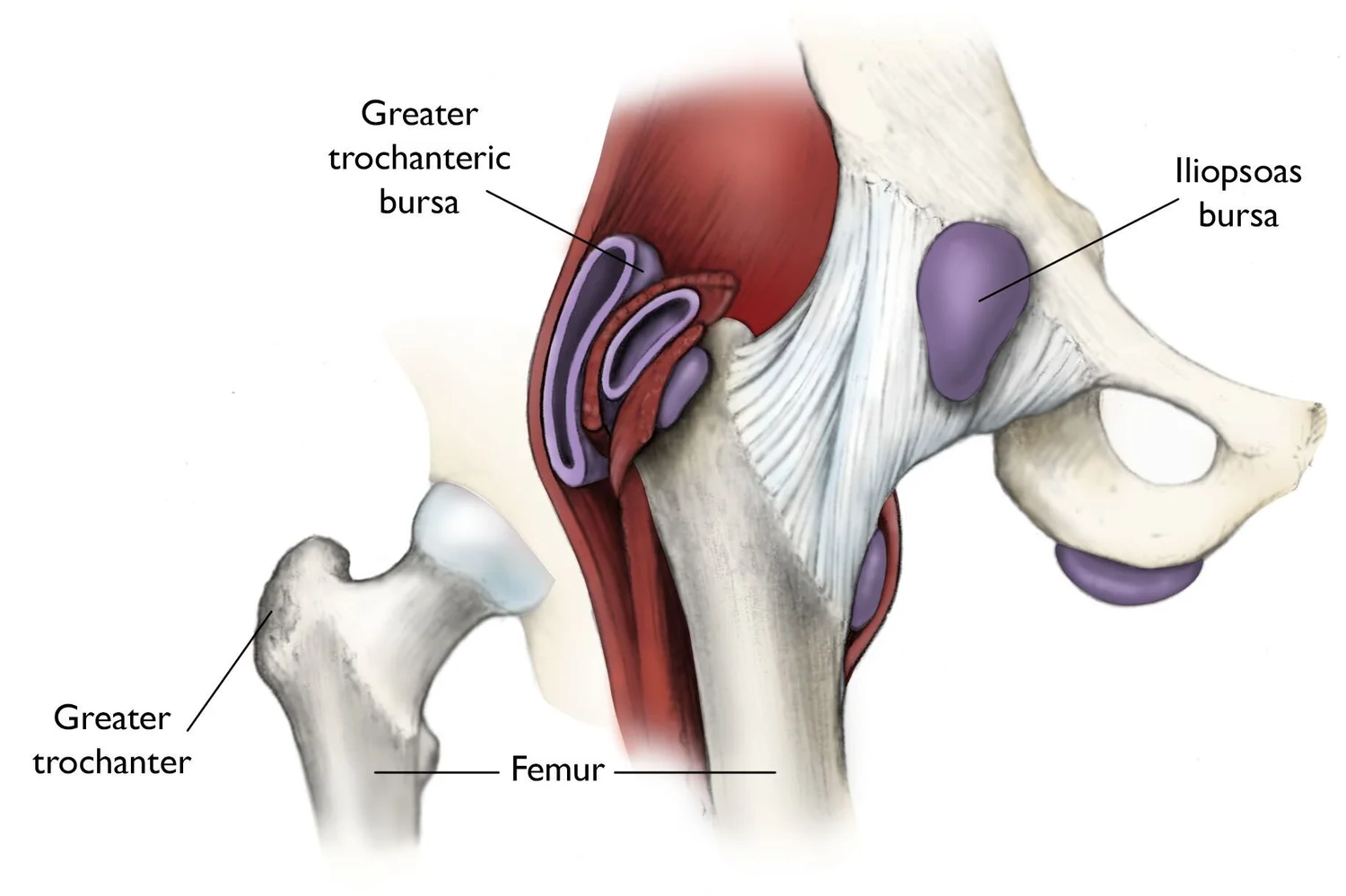
Gluteal tendinopathy refers to irritation or degeneration of the gluteus medius and/or gluteus minimus tendons where they attach to the greater trochanter — the bony point on the side of your hip.
It's one of the most common causes of outer hip pain, especially in women over 40, runners, and people who spend long hours sitting or standing on one leg.
For years, any pain on the side of the hip was labelled trochanteric bursitis, implying inflammation of the bursa — the small fluid sac that cushions the hip joint.
But modern research and imaging tell a different story:
That's why the term "Gluteal Tendinopathy" has replaced "trochanteric bursitis" — it reflects what's actually happening at the tissue level.
| Old Thinking: "Trochanteric Bursitis" | Modern Approach: "Gluteal Tendinopathy" |
|---|---|
| 🔹 Assumed inflammation was the main problem | 🔹 Recognizes tendon degeneration and overload as the true cause |
| 🔹 Emphasis on rest, NSAIDs, and corticosteroid injections | 🔹 Focus on graded loading, strength training, and patient education |
| 🔹 Passive treatments (ice, ultrasound, heat) | 🔹 Active rehabilitation (targeted gluteal loading, movement retraining) |
| 🔹 Relief is often short-lived; pain may recur | 🔹 Builds tendon capacity and long-term resilience |
| 🔹 Avoids movement | 🔹 Encourages smart, progressive loading |
Avoid positions that compress the tendon — like crossing legs, sitting with knees together, or lying directly on the sore side.
Progressive loading of the gluteus medius and minimus improves tendon strength and function. Exercises often start with isometrics and build toward functional loading.
Understanding tendon recovery is crucial — tendons respond best to controlled load, not rest. Patience and consistency are key.
A single corticosteroid injection or shockwave therapy can help reduce pain temporarily, but should complement — not replace — structured rehab.
"Tendons don't like total rest — they recover best through smart, progressive loading."
In clinic, I often see patients who've struggled for months with "hip bursitis" that never quite settled. Once we shift focus from inflammation to tendon health, recovery begins to make sense.
The goal is not rest — it's rebuilding strength, balance, and movement confidence.
This updated understanding helps patients take an active role in their healing — and that's where real change happens.
Categories: Hip Pain, Tendinopathy, Evidence-Based Practice Tags: #glutealtendinopathy, #hippain, #tendinopathy
Phone: +91 8148 66 5479
Email: m7physiocentre@gmail.com
Address: Anna Nagar, Chennai
Hours: Mon-Sat: 9:00 AM - 7:00 PM